Close to the heart – echocardiography in times of pandemic
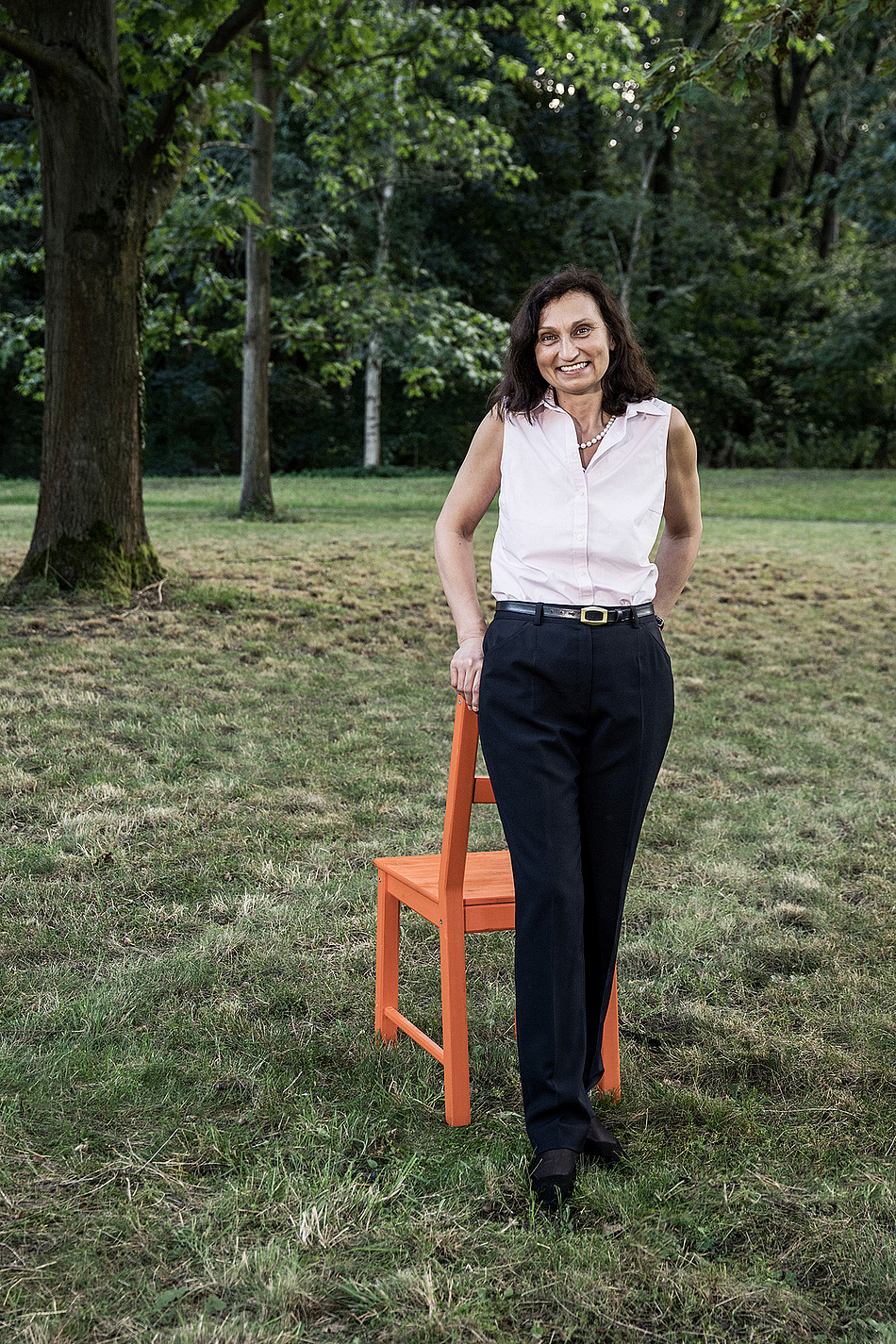
Dr. Ursula Wilkenshoff has been in charge of echocardiography at the Benjamin Franklin Campus of the Charité for more than ten years. In addition to her clinical activity, the experienced senior physician is supported by the Charité Foundation as a BIH Clinical Fellow. She has been tracking the difference between male and female hearts for many years. In September 2020, we visited Dr. Wilkenshoff at her workplace in the clinic to talk to her not only about her project, but also about her personal experiences during the COVID-19 pandemic.
Dr. Wilkenshoff, you have been working on the echocardiography method since your doctorate. What is behind it and why do we need it?
Echocardiography is an ultrasound examination of the heart. It is a wonderful way to look into the heart, Allowing us to scan it from all sides, determine its exact size and investigate its function. Are there heart defects? Are the heart valves still opening properly? How thick is the heart wall? We can see all of this with ultrasound very clearly – much better than a few decades ago, by the way. The technical development of this method is phenomenal. The imaging is now so differentiated that we can accompany the surgeons and cardiologists during heart surgery and intervention. Unlike X-ray, ultrasound does not result in radiation exposure, which means that younger patients, children or even pregnant women can be examined without a problem. Some of our patients, such as those with water accumulation in the heart, for example, come to us daily. The heart is not damaged during the examination. Another big advantage is that our devices are quite small. We can bring portable echocardiography devices to the wards. Emergency medical carts are equipped with these devices and general practitioners like to take them along on house calls.
From which wards do most patients come to you?
First of all, of course, the cardiac wards. But we also have numerous patients coming to us from other wards. From neurology, for example, we often see stroke patients and cancer patients from hematology and oncology. Although we have very good and advanced chemotherapies, some have the disadvantage that they can damage the heart. We accompany these patients during and after chemotherapy. We also frequently examine patients from the admission ward. For example, if a patient with breathing difficulties is admitted and the ECG [editor's note: electrocardiogram] does not show anything striking, then echocardiography is usually the next diagnostic tool to be used.
Earlier, you mentioned the size of the heart, which you are able to determine with great precision. Is it good or bad to have a big heart?
Actually, it is said that it a good person has a big heart, but, from the point of view of echocardiography, having a big heart is not such a good thing. An enlarged heart always means that it can no longer hold its structure because the heart fibers have been damaged either by a heart attack or by inflammation. As a result, it is coming apart.
Is an athlete's heart, which is well trained and therefore has more volume, exempt from this problem?

Funding program
BIH Clinical Fellows
Funding period
2017 – 2022
Project title
Gender-Specific Aspects in Echocardiography
Research area
Cardiology
Institution
Charité – Universitätsmedizin Berlin
Since 1998
Senior physician and Head of Echocardiography, Charité – Universitätsmedizin Berlin, Benjamin Franklin Campus
Since 1999
Specialist for Internal Medicine
1979 – 1992
Medical studies and doctorate in Berlin
It is to some extent, but athletes should also be careful. Nowadays, more and more athletes are being accompanied by echocardiography in addition to the ECG. Care should be taken to ensure that the heart does not become too big and hypertrophy does not develop. In the long term, the heart cannot tolerate this condition well. If it gets bigger and stronger, the pumping function will suffer at some point. With the help of an echocardiogram, this problem can be detected at an early stage. I am therefore pleased that this method is also finding wider applications in sports medicine.
As part of your clinical fellowship, you are studying gene-specific diagnostic imaging in echocardiography. Why is this important?
"Women's hearts beat differently than men's hearts" – We hear this more and more in the media nowadays. And in fact, many studies have shown that the hearts of women react slightly differently to diseases than the hearts of men and that the symptoms of these diseases are also different. A good example is the heart attack. We now know that the symptoms of a heart attack often are different in women than in men – not presenting through pressure in the chest and pain that radiates into the left arm, for example, but rather through diffuse pain in the abdomen and back and nausea. To date, heart attacks in women are therefore often not detected in time. Men are still the norm here, which we should change.
Do you have any idea why the symptoms are different between men and women? Is this a matter of sensitivity or can that be explained on the molecular level?
To this day, we do not know exactly. What is interesting in this context, however, is that women and men treat stress differently. You may have heard of stress-induced Takotsubo cardiomyopathy, that is, broken heart syndrome. This condition is much more common in women than in men. If the woman suddenly experiences extreme stress, e.g. due to a very tragic event in her life, this situation can actually cause damage to the heart, similar to a heart attack. In the echocardiogram, this "broken heart" can be clearly identified. In the tip, the heart is fully expanded and the pumping function is weakened. The heart is under enormous pressure; it is stretched to the point of bursting, and some patients die from this condition. The good thing about this disease, however, is that the heart actually recovers as soon as the stress subsides. Most of the time, the heart returns to normal again after a few weeks.
You want to make gender-based assessment clinical routine. What is the situation now?
The fact that male and female hearts differ, for example, in size, and that different standard values must be applied in diagnosis is now generally known. Numerous studies have been conducted on this circumstance, I have written an echocardiography manual myself with all the different standard values, and the guidelines have also taken it into account in the meantime. Nevertheless, it is sometimes a long step from what one should do ideally to the actual routine. This is where my project starts. I work closely with an IT specialist, with whom I am developing a digital entry mask in which the corresponding standard values are stored on a gender-specific basis. In case of pathological deviation, a color signal will appear so that the deviation can be detected immediately. This tool especially helps younger colleagues come to the correct diagnosis, benefiting not only women, but also various other patients due to the inclusion of gender, height and weight. For a dainty person or a teenager, different standard values must be set than for a bodybuilder. We coordinate closely with the other Charité campuses and are constantly developing the mask so that other useful parameters such as the wall thickness or the function of the different heart cavities can also be entered.
Let us now move on to a very topical issue: How did the COVID-19 pandemic affect your daily hospital life?At the very beginning, the impact was massive. We were entering truly uncharted territory and there was great uncertainty. We saw the serious course of the disease in Italy and we did not know how to handle patients. All examinations of patients who were not life-threateningly ill were canceled. Echocardiographic examinations were kept to a minimum. Since we could not maintain a sufficient distance from the patients during our examinations, we used masks from the very beginning, although it was not yet clear whether they were any use at all. After this initial shock phase, we developed standard operating procedures (SOPs) for all campuses of the Charité.
How do we behave when a patient comes in with a COVID diagnosis? What do we do if an infection is suspected and how do we handle a patient who has not yet had a test? How do we examine them, do we examine them at all, and where do we examine them? These were all issues that urgently needed to be resolved. With the SOPs, we therefore had something in hand with which we could get our bearings. Colleagues who had ever worked in the intensive care unit were once again trained in the use of ventilators. And doctors were kept ready for these wards and for the COVID wards that were then set up. The equipment of these wards and the deployment of staff went really fast. This was an intense time when new information was being discovered every day.
Do you now have to deal with COVID-19 patients in your clinical practice?
Yes, under very special precautions, we examine the patients in the COVID-19 ward. We have also had some serious cases. Once they have recovered and tested negative three times, they come directly to us for echocardiography. I have seen a number of patients who are really seriously affected. A colleague from my personal environment was also infected, which deeply affected me. She was so seriously ill that she had to be ventilated and then came in for an echocardiogram to see whether her heart function was impaired. Her heart pump function was good luckily – as has been the case with many other COVID-19 patients. Nevertheless, as a physically fit person, she was so weak that she could no longer move from her wheelchair to the bed. Her kidneys are affected, she has headaches and her memory is impaired. I was quite shocked.
Do patients come to you who did not have to be given intensive medical care before? After all, we also read a lot about affected persons who did not really recover entirely after a rather mild infection.
Yes, I've seen some of that. They are often referred to us by their general practitioners to see whether their fatigue may be due to impaired heart pump function. But that is not the case. There were no major changes of the cardiac performance in the patients I saw. Cardiac strength was not affected. One thing is interesting, though. In the medical field, a distinction is made between systole, as the heart contracts, and diastole, as the heart relaxes. During contraction, these patients had no major limitations. The diastole, however, was striking. The heart had problems with relaxation, which, by the way, is something that occurs more frequently in women than in men. We echocardiographers need to be careful to focus not only on systole, that is, how much the heart pumps, but also to look at how the heart relaxes.
The last few months have probably been anything but relaxing. How did the first pandemic phase affect you and your personal environment?
We were in turmoil. We thought of our families and friends. We even considered whether we should stay overnight at the hospital due to contact with patients. One cannot deny that it was a time of particular uncertainty and burden. A big help was that we had and still have such a wonderful cohesion within the team. Despite the cancellation of almost all in-person meetings, courses and further education, we in the Echocardiography department and in the entire clinic have grown together in the time of social distancing. Everyone has tried to do their best to manage the situation together. I am very happy and grateful about that.
September 2020 / Marie Hoffmann